Unicompartmental Knee Replacement

An overview:
Partial knee replacement or Uni knee replacement is a treatment option that replaces (or resurfaces) only the damaged portion of the knee while conserving knee ligaments and unaffected cartilage.
Knee osteoarthritis may occur in any one of the three compartments that make up the knee joint. The medial compartment is by far the most frequent site of osteoarthritis of the knee, with the disease occurring less frequently in the lateral compartment. Isolated patellofemoral osteoarthritis is even more uncommon.
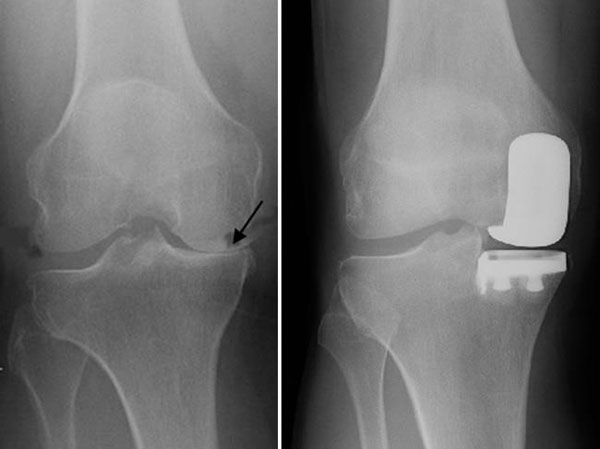
Patients with uni-compartmental knee arthritis have osteoarthritis in only one section or compartment of the knee. In cases where non-operative therapies do not provide sufficient symptom relief, surgeons can remove damaged cartilage and bone in the diseased area only, while preserving the ligaments that help support the knee joint as well as the cartilage in the unaffected areas of the knee.
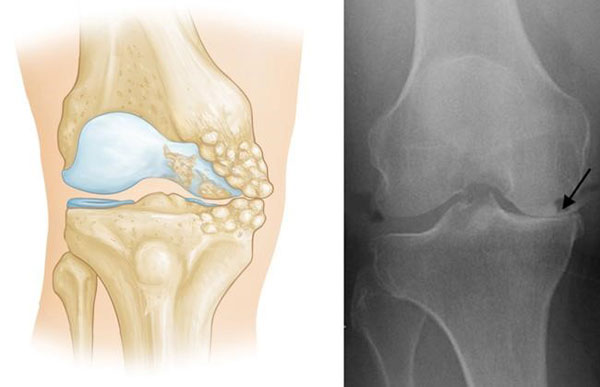
The Uni Knee replacement takes the place of the damaged area of the knee, leaving the other compartments intact.
Between 10-15% of patients who present with knee osteoarthritis may be suitable for a uni-compartmental knee replacement.
Partial knee replacement is appropriate for patients with arthritis that is confined to a single compartment of the knee and is generally restricted to patients who are not morbidly obese.
The surgery is not appropriate for patients with marked stiffness in the knee or those with a significant angular deformity or significant instability due to ligament damage.
Patients with inflammatory arthritis (like rheumatoid arthritis) are not candidates for a uni-compartmental replacement because inflammatory-type arthritis typically involves the entire joint.
Patient selection is critical in deciding who is suitable for a uni-compartmental knee replacement and with good patient selection, the results are excellent.
The expectation is that a uni-compartmental knee replacement may well last up to 20 years. Dr Solomon’s registry data has shown that his revision rate is 2.5% at 10 years. Revision to a total knee replacement is possible after a uni-compartmental knee replacement. The outcomes of revision from a uni-compartmental to a total knee replacement are similar to revisions from a total knee replacement to another totally replacement.
The major advantage of a uni-compartmental knee replacement over a total knee replacement is the following:
- Early recovery compared to TKR
- Far less invasive surgical process
- Feeling that the knee feels more like a “normal knee” compared to a TKR.
- Preservation of the native patellofemoral and lateral compartment and cruciate ligaments.
- Generally a better range of motion/flexibility.
- Easier to kneel compared to a TKR.
- Usually an easier revision to a TKR compared to revising a TKR to another TKR.
Surgery is performed under a general anaesthetic combined with a local adductor nerve block and further local anaesthetic that is placed around the knee joint.
The surgery involves a small incision over the medial (inner) side of the patella (kneecap). The affected medial compartment is then entered and the worn out bone/cartilage is reshaped and prepared to receive the artificial joint. Accurate sizing is insured by using trial implants before the definitive implants are cemented in place. An appropriately sized polyethylene insert (new cartilage) is placed on the tibial component.
The wound is again infiltrated with local anaesthetic prior to closure with absorbable sutures. An ice compression bandage is placed around the knee and patients are encouraged to mobilise on the same day of surgery.
Hospital stay is usually one or two nights and patients are discharged home when comfortable with an outpatient physiotherapy program. Patients do not require inpatient rehab as there is no advantage to this. Outpatient physiotherapy will achieve the same outcome and patients are far better off at home than remaining in a hospital environment.
The dressing remains on the knee for a period of two weeks and then is removed. There are no stitches that require removal when the dressing comes off.
Patients are given pain relief medication upon discharge. It is also important to take 100 mg of aspirin daily for a period of two weeks following the surgery. This is to prevent deep vein thrombosis. Mobilisation is key to preventing deep vein thrombosis and I encourage patients to walk or use an exercise bike as soon as practical.
Driving is usually possible after two weeks provided you are not taking heavy analgesics.
Returning to work after two or three weeks is usually the norm.
It takes about 8 to 10 weeks until the knee feels relatively comfortable to allow exercise walking, golf and tennis. There will however be at least 3 to 4 months of ongoing recovery following this period.
It is normal for the knee to remain warm and swollen for the first two months.
It is normal to occasionally feel or hear a click in the knee as this is simply the metal on plastic sound.
Robotic surgery:
At this stage, there is no evidence that the use of a robotic arm is any better than a surgeon who performs a well done uni-compartmental replacement using sound surgical techniques.
Complications following a uni-compartmental knee replacement:
Early complications are rare. There are small risks with any surgical procedure requiring an anaesthetic and the anaesthetist will discuss the anaesthetic with you prior to surgery.
Risks of unicompartmental knee replacement surgery are low 1-2%).
It is very common to feel a little bit of altered sensation/numbness on the outer side of the wound. This is usually present in all patients who require a uni-compartmental (or total knee) replacement. It is simply a minor branch of a skin nerve that gets in the way of the incision that can leave a number patch on the side of the wound. Over time, this numbness tends to improve.
The main risks/complications that can occur in uni-compartmental knee replacement surgery are as follows:
- Bleeding
- Infection
- Deep vein thrombosis and rarely Pulmonary Embolus
- Stiffness
- Fracture
- Ongoing pain
- Nerve or vascular injury
- Long-term wear of the polyethylene
- Long-term loosening of the implant
- Eventual wear and development of arthritis in the unaffected compartments.
Take home message:
The most important determinant of a good long-term outcome for a uni-compartmental knee replacement is careful patient selection and surgery performed by an experienced and skilled orthopaedic surgeon.
Rehabilitation following Uni Knee Replacement:
Many patients DO NOT require formal inpatient rehabilitation and can be discharged home with outpatient physiotherapy and a home based excersise program. Studies have conclusively shown that there is NO difference in outcomes between inpatient and outpatient rehab.
There is a false perception that by not going to inpatient rehab your result will be inferior. This is simply NOT TRUE and many published studies have proven that home discharge is as good.
I encourage patients to go home following surgery however there are patients who benefit from inpatient rehab when home circumstances are not ideal or where extra medical attention is required.
ANTIBIOTIC POLICY FOR PROCEDURES FOLLOWING JOINT REPLACEMENT
The risk of getting an infection in your replaced joint is extremely rare following routine procedures such as dental work and colonoscopies.
DENTAL procedures:
For routine dental cleaning after joint replacement surgery there is no need to take antibiotic prophylaxis. For major dental work within 3 months after a joint replacement ( such as root canal etc) I recommend a single dose of 2gm amoxicillin 1 hour before provided you are not allergic to amoxil. It is not necessary to take antibiotics for any dental work after 3 months provided your health is reasonably good.
COLONOSCOPY, Prostate, Bladder or Gynaecological procedures after joint replacement :
Routine colonoscopy without any major biopsies or risk of bleeding do not require prophylactic antibiotic cover.
Surgery to the bladder, bowel, gynaecological and prostate surgery require a single intravenous antibiotic dose that is administered by the surgeon at the time of the procedure. Please advise them that you have a joint replacement.